Navigating Medical Aid: Is Chiropractic Care Included?
Understanding Medical Aid Coverage for Chiropractic Care
Does medical aid cover chiropractic care? The answer depends on your specific insurance plan, location, and the type of treatment you need. Here’s what you need to know:
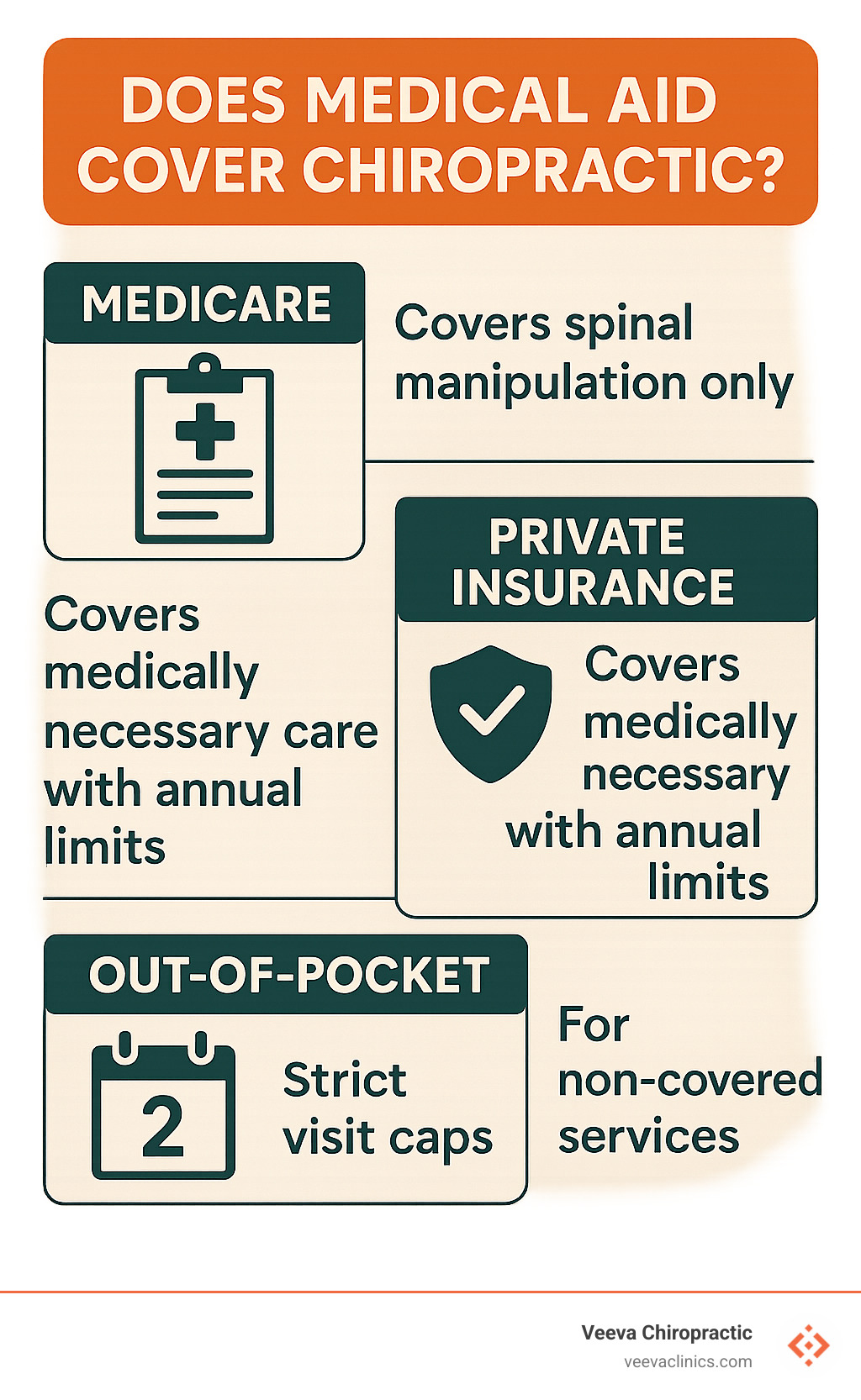
Quick Coverage Overview:
- Medicare Part B: Covers spinal manipulation for vertebral subluxation only
- Private Insurance: Most plans cover medically necessary chiropractic care with limits
- Medicaid/Medi-Cal: Limited coverage (typically 2 visits per month for adults)
- South African Medical Schemes: Chiropractic is an optional benefit, not a PMB
- Coverage Requirements: Medical necessity, licensed providers, specific diagnosis codes
Around 80% of people in the U.S. experience back pain at some point in their lives, making chiropractic care a popular treatment option. Yet many people avoid seeking help because they’re unsure about insurance coverage.
The reality is that most health insurance plans do cover chiropractic services when they’re deemed medically necessary. However, the specifics vary dramatically between different types of medical aid programs.
Under the Affordable Care Act, chiropractic care is considered an essential health benefit, but insurance companies still set their own rules about visit limits, referral requirements, and which services they’ll pay for. Some plans cap you at 12 visits per year, while others allow unlimited visits as long as they’re medically necessary.
The key is understanding your specific plan’s rules before you need care. This guide will walk you through exactly what different medical aid programs cover, what they don’t, and how to steer the system to get the care you need without surprise bills.
Find more about does medical aid cover chiropractic:
What Exactly Is Chiropractic Care & Who Can Benefit?
Chiropractic care focuses on diagnosing and treating musculoskeletal disorders, particularly those affecting the spine. At its core, chiropractic treatment involves manual manipulation of the spine and other joints to improve function and reduce pain.
The conditions we commonly treat with chiropractic care include:
- Back pain and sciatica – affecting millions of Americans annually
- Neck pain and whiplash – often from auto accidents or poor posture
- Headaches and migraines – frequently stemming from cervical spine issues
- Joint pain in shoulders, hips, and extremities
- Pregnancy-related discomfort – as the body adapts to changes
- Pediatric conditions like scoliosis or developmental issues
Research shows that chiropractic care can be highly effective for these conditions. Scientific research on chiropractic care for back pain demonstrates that manual therapy often provides better outcomes than medication alone for many musculoskeletal conditions.

Core Techniques & Adjunctive Therapies
Modern chiropractic care extends far beyond the traditional “crack” that people often associate with adjustments. At our clinics, we use a comprehensive approach that includes:
Primary Chiropractic Techniques:
- Spinal manipulation – precise adjustments to restore joint mobility
- Soft-tissue therapy – myofascial release and trigger point therapy
- Therapeutic exercise – strengthening and mobility programs
- Postural correction – ergonomic education and workplace modifications
Adjunctive Therapies:
- Electrical muscle stimulation – for pain relief and muscle recovery
- Acupuncture – complementary pain management technique
- Massage therapy – integrated soft-tissue treatment
- Naturopathic support – holistic wellness approaches
This multi-modal approach is particularly effective for auto accident and workplace injuries, which are specialties at our Oregon clinics. By combining these techniques, we can address both the immediate symptoms and underlying causes of musculoskeletal dysfunction.
Does Medical Aid Cover Chiropractic?
The short answer is: usually yes, but with important limitations. The coverage landscape varies significantly depending on your specific type of medical aid.
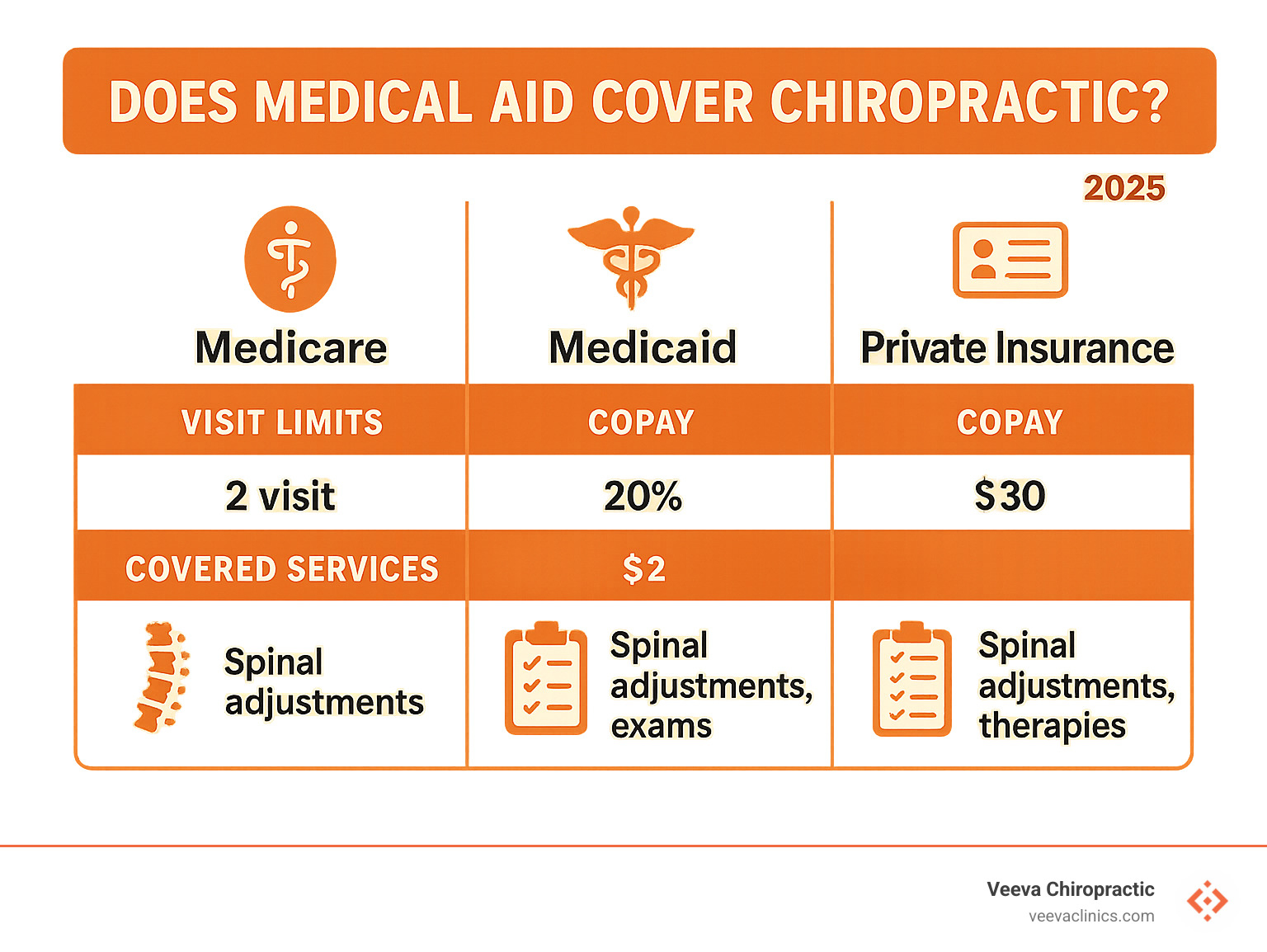
Medicare Part B Coverage:
Medicare covers only manual manipulation of the spine by a chiropractor to correct a vertebral subluxation. This means Medicare will pay for spinal adjustments, but won’t cover other services like X-rays ordered by chiropractors, massage therapy, or acupuncture (except for chronic low back pain). If you have Medicare Part B, you’ll pay 20% of the cost of a chiropractic adjustment after meeting your deductible.
Private Health Insurance:
Most health insurance plans cover chiropractic services that are deemed medically necessary, as long as they’re performed by a licensed chiropractor. Under the Affordable Care Act, it’s mandatory for compliant health plans to cover chiropractic care services, but the exact amount of coverage varies depending on your state and insurance provider.
Medicaid Programs:
Coverage varies dramatically by state. For example, Medi-Cal (California Medicaid) covers up to 2 chiropractic visits per calendar month for most adults, with broader coverage for children under 21, pregnant individuals, and nursing-facility residents. The reimbursement rate is $16.72 for CPT codes 98940, 98941, and 98942.
For more detailed information about Medicare coverage, check out the Scientific research on Medicare chiropractic policy.
Does medical aid cover chiropractic for adults vs children?
There’s a significant difference in coverage between adults and children, particularly under Medicaid programs.
Adult Coverage:
- Most adults are limited to 2 chiropractic visits per calendar month under Medi-Cal
- Services must be provided at Federally Qualified Health Centers (FQHCs) or Rural Health Clinics (RHCs)
- Only manual manipulation of the spine for sprain, strain, or dislocation is covered
- Maintenance care is explicitly excluded
Pediatric Coverage:
Children under 21 receive much more comprehensive coverage under the Early and Periodic Screening, Diagnostic and Treatment (EPSDT) program. This federally mandated benefit requires unlimited medically necessary services for Medicaid beneficiaries under 21, without the facility restrictions that apply to adults.
Special Exemptions:
- Pregnant individuals can receive services using modifier TH without the standard monthly limits
- Nursing facility residents are exempt from optional benefit exclusions using modifier KX
- Continuing care patients transitioning from pediatric to adult coverage may use modifier GY
Does medical aid cover chiropractic in South Africa under PMBs?
In South Africa, the situation is quite different. Chiropractic care is generally not covered under Prescribed Minimum Benefits (PMBs). PMBs cover approximately 270 conditions including emergencies, chronic diseases, and specific diagnosis-treatment pairs, but chiropractic services are typically classified as optional benefits.
This means:
- Medical schemes are not legally required to cover chiropractic care
- Coverage depends on your specific scheme and plan level
- You may need to use Designated Service Providers (DSPs) if coverage is available
- Co-payments and annual limits often apply
The Medical Schemes Act of 1998 governs these benefits, and while schemes may choose to offer chiropractic coverage, it’s not mandated like the 25 chronic conditions on the official Chronic Disease List.
What Services Are Typically Covered—And What’s Not?
Understanding exactly which chiropractic services are covered can save you from unexpected bills. Here’s the breakdown:
Typically Covered Services:
- Manual spinal manipulation (CPT codes 98940-98942)
- Initial examination and consultation
- Follow-up visits for ongoing treatment
- Diagnostic services ordered by a medical doctor
- Physical therapy when prescribed by a physician
Commonly Excluded Services:
- Maintenance care – ongoing treatment without active symptoms
- X-rays ordered by chiropractors (though MD-ordered X-rays may be covered)
- Massage therapy provided by chiropractors
- Acupuncture (except for chronic low back pain under Medicare)
- Nutritional counseling and supplements
- Orthotics and supports above plan limits (often $50 maximum)
The key distinction is between “medically necessary” care and “wellness” or “maintenance” care. Insurance companies typically only cover treatment that addresses specific symptoms or conditions, not ongoing preventive care.
For billing purposes, providers must use approved ICD-10-CM diagnosis codes in the primary position to avoid claim denials. The most commonly covered diagnoses include:
- Cervical disc disorders (M50.11-M50.13)
- Lumbar disc disorders (M51.14-M51.17)
- Dorsalgia (M54.17)
- Cervicalgia and lumbar pain (M54.31-M54.32)
Navigating Limits, Costs & Paperwork
Successfully using your chiropractic benefits requires understanding the administrative requirements and cost-sharing structures of your plan.
Common Visit Limits:
- Medicare: No limit on visits, but each must be medically necessary
- Private insurance: Typically 12-30 visits per calendar year
- Medi-Cal: Maximum of 2 visits per calendar month
- Medicare Advantage: May offer up to 30 visits per year with $10 copays
Cost-Sharing Structures:
- Medicare Part B: 20% coinsurance after deductible
- Private PPO plans: Usually $20-40 copays or 20% coinsurance
- HMO plans: Often require referrals but lower copays
- High-deductible plans: Full cost until deductible is met, then coverage begins
Prior Authorization Requirements:
Some plans require Treatment Authorization Requests (TARs) for:
- Services exceeding standard visit limits
- Certain diagnostic procedures
- Specific treatment modalities
- Continuing care beyond initial treatment period
For more information about managing costs, check out our guide on costs without insurance.
Verifying Benefits & Finding Providers
Before your first visit, it’s crucial to verify your specific benefits to avoid surprises. Here’s how:
Step 1: Check Your Plan Documents
- Review your Summary of Benefits and Coverage
- Look for “chiropractic” or “alternative medicine” sections
- Note any annual or per-visit limits
Step 2: Call Your Insurance Company
Use this phone script: “I need to verify my chiropractic benefits. Can you tell me my copay, any deductible requirements, visit limits, and whether I need a referral?”
Step 3: Use Online Tools
- Log into your insurance company’s member portal
- Use provider directory searches
- Check eligibility and benefits online
Step 4: Verify Provider Network Status
- Confirm your chiropractor is in-network
- For Medi-Cal, verify the provider is at an FQHC or RHC
- For Medicare Advantage, check the ASH network if applicable
For Oregon residents, we’ve created a detailed guide about insurance coverage in Oregon that covers state-specific requirements.
What If Your Plan Says No?
Don’t panic if your initial claim is denied or if your plan doesn’t cover chiropractic care. You have several options:
Alternative Coverage Sources:
- Workers’ compensation – if your condition is work-related
- Auto insurance PIP – for accident-related injuries
- Supplemental insurance – chiropractic-specific riders
- Health Savings Accounts – tax-advantaged payment method
Self-Pay Options:
- Many clinics offer cash-pay discounts
- Payment plans may be available
- Discount programs like those offered through ASH Plans
- Package deals for multiple visits
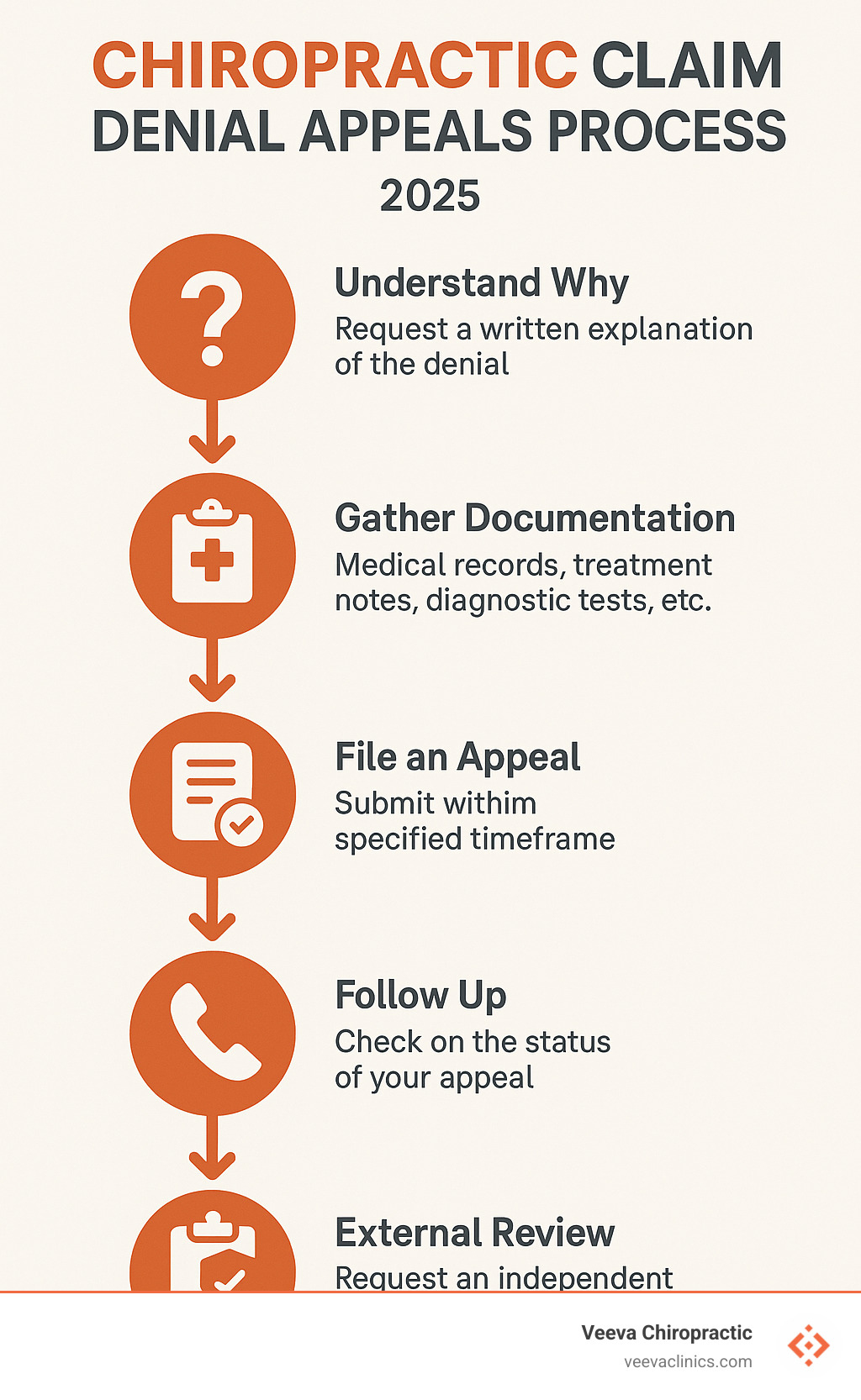
Appeal Process:
- Request a written denial explanation
- Gather supporting documentation from your chiropractor
- Submit a formal appeal with medical necessity justification
- Follow up within the specified timeframe
- Consider external review if internal appeals fail

Frequently Asked Questions about Does Medical Aid Cover Chiropractic
How many chiropractic visits will my medical aid pay for each year?
The number of covered visits varies significantly by plan type:
- Medicare: No annual limit, but each visit must be medically necessary to treat vertebral subluxation
- Private insurance: Typically 12-30 visits per calendar year, depending on your plan
- Medi-Cal: 2 visits per calendar month for adults (24 per year maximum)
- Medicare Advantage: Often 30 visits per year with participating providers
- Children under 21: Unlimited visits if medically necessary under EPSDT
These limits apply to covered visits only. You can always pay out-of-pocket for additional care if needed.
Do I need a referral from my primary doctor before seeing a chiropractor?
This depends on your insurance type and state regulations:
No Referral Required:
- Medicare Part B (original Medicare)
- Most PPO plans
- Oregon residents (chiropractors are recognized as primary care providers)
- Fee-for-service Medicaid in most states
Referral May Be Required:
- HMO plans often require primary care referrals
- Some Medicare Advantage plans
- Certain Medicaid managed care plans
- Workers’ compensation cases
Special Cases:
- Massage therapy typically requires a referral when insurance is involved
- Chiropractors can prescribe massage therapy treatments
- Some plans require referrals for certain services but not others
What should I do if my chiropractic claim is denied?
Claim denials are frustrating but often reversible. Here’s your action plan:
Step 1: Understand Why
- Request a written explanation of the denial
- Common reasons include: wrong diagnosis codes, non-covered services, visit limits exceeded, or lack of medical necessity documentation
Step 2: Gather Documentation
- Medical records showing your condition
- Treatment notes from your chiropractor
- Any relevant imaging or diagnostic tests
- Documentation of functional improvement
Step 3: File an Appeal
- Submit a formal appeal within the specified timeframe (usually 60 days)
- Include all supporting documentation
- Have your chiropractor write a letter explaining medical necessity
Step 4: Follow Up
- Insurance companies must respond within 30 days for urgent appeals
- Non-urgent appeals may take up to 60 days
- Keep records of all communications
Step 5: External Review
- If internal appeals fail, request an external review
- This is often free and conducted by independent medical reviewers
- Contact your state insurance commissioner if needed
Conclusion
Understanding does medical aid cover chiropractic care doesn’t have to be overwhelming. While coverage varies significantly between different types of medical aid programs, most plans do provide some level of chiropractic benefits when care is medically necessary.
The key takeaways are:
- Medicare covers spinal manipulation for subluxation only
- Private insurance typically covers 12-30 visits annually
- Medicaid programs have strict limits but broader coverage for children
- South African medical schemes treat chiropractic as optional
- Always verify your specific benefits before treatment
At Veeva Chiropractic, we understand how complex insurance navigation can be. That’s why our team handles benefit verification for you, ensuring you understand your coverage before beginning treatment. Whether you’re dealing with auto accident injuries, workplace trauma, or chronic pain conditions, we work with your insurance company to maximize your benefits.
Our integrated approach combining chiropractic care, acupuncture, naturopathic medicine, and massage therapy means we can often provide comprehensive treatment within your insurance benefits. With locations throughout Oregon in Beaverton, Happy Valley, Hillsboro, Gresham, Portland, Salem, and Woodburn, plus Vancouver, Washington, we’re here to help you steer both your pain and your insurance coverage.
Don’t let insurance uncertainty prevent you from getting the care you need. Contact us today to verify your benefits and start your journey toward better health.
For more information about our comprehensive approach to care, visit our chiropractic services page.