Spinal Solutions: Understanding Medi-Cal’s Chiropractic Coverage
Navigating Chiropractic Coverage Under Medi-Cal — and How It Compares to Coverage in Oregon & Washington
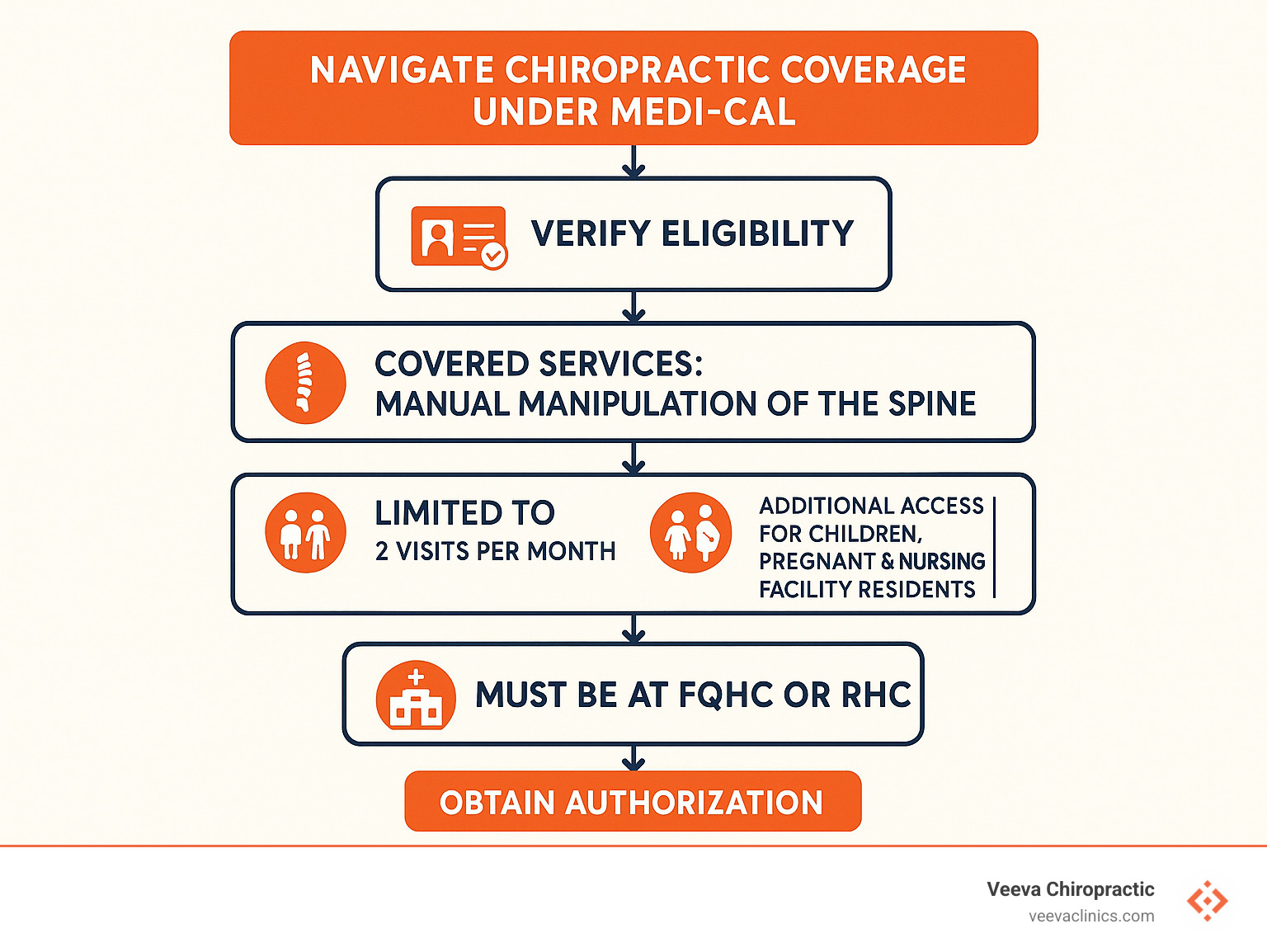
Does Medi-Cal cover chiropractic care? Yes, but with specific limitations.
Because many of our readers visit Veeva Chiropractic clinics in Oregon and Southwest Washington, we’ve also sprinkled in quick comparisons to the Oregon Health Plan (OHP) and Washington’s Apple Health program so you can see how coverage differs where we actually practice.
Key take-aways for Medi-Cal members:
-
Covers up to 2 chiropractic visits per calendar month
-
Only covers manual manipulation of the spine (CPT codes 98940-98942)
-
For most adults, services must be provided at Federally Qualified Health Centers (FQHCs) or Rural Health Clinics (RHCs)
-
Children under 21, pregnant individuals, and nursing-facility residents get broader access
-
No coverage for maintenance care, X-rays ordered by chiropractors, or massage therapy
By comparison, Oregon Health Plan allows chiropractic manipulation when it is referred or ordered by an in-network primary-care provider, and Washington Apple Health currently limits routine chiropractic benefits to children, pregnant people, and a handful of special circumstances. (We’ll dive deeper into these regional differences later in the article.)
If you’re a California resident researching Medi-Cal, the details below will help you open up the benefits you’re entitled to. If you live in Oregon or Washington and visit a Veeva clinic, keep an eye out for the OHP and Apple Health call-outs to see how your coverage stacks up.
Does Medi-Cal Cover Chiropractic Care?
Yes, Medi-Cal does cover chiropractic care – but with several important limitations you should understand before scheduling your first appointment.
When Medi-Cal covers chiropractic treatment, it’s specifically for manual manipulation of the spine to fix subluxations (partial misalignments of your spinal joints). Your chiropractor must document that this treatment is medically necessary – not just maintenance care – for it to be covered.
For most adults (21 and older), there’s a crucial detail to know: you’ll typically need to receive chiropractic care at specific facilities:
- Federally Qualified Health Centers (FQHCs)
- Rural Health Clinics (RHCs)
- Indian Health Service facilities
This FQHC/RHC requirement exists because California’s Welfare and Institutions Code classified chiropractic as an “optional benefit” with specific limitations on where services can be provided.
“I was confused at first when my regular chiropractor couldn’t accept my Medi-Cal,” says Maria, a 45-year-old with chronic lower back pain. “My primary care doctor explained the FQHC rule and referred me to a qualified clinic. It took an extra step, but the pain relief was absolutely worth it.”
For most members, Medi-Cal limits coverage to just two chiropractic visits per month. This cap is actually shared across several therapy services – including acupuncture, audiology, occupational therapy, and speech therapy. So if you use one chiropractic visit and one acupuncture visit in the same month, you’ve reached your monthly limit.
Your coverage may vary depending on which type of Medi-Cal you have:
Fee-for-Service Medi-Cal follows the standard rules with the FQHC/RHC requirement and two-visit monthly cap.
Managed Care Plans might offer better access. Some plans contract with American Specialty Health (ASH) networks to provide chiropractic services beyond just FQHCs for members with back and neck pain.
Scientific research consistently supports spinal manipulation for certain conditions, which is why Medicare also covers similar services, though with their own set of limitations.
Does Medi-Cal Cover Chiropractic Care for Adults vs. Children?
There’s a world of difference between how Medi-Cal covers chiropractic care for adults versus children.
For adults 21 and older, the restrictions are significant – two visits monthly, services generally limited to FQHCs or RHCs, and coverage only for medically necessary treatment (not maintenance care).
Children under 21, however, have much better coverage thanks to the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) benefit. This federally-mandated program requires Medi-Cal to provide all medically necessary services to correct or improve physical conditions for beneficiaries under 21 – even if those services aren’t covered for adults.
For kids, this means:
- No strict monthly visit limits when care is medically necessary
- Services available at any Medi-Cal provider, not just FQHCs/RHCs
- More comprehensive coverage for both prevention and treatment
“The difference in coverage for my pediatric patients is dramatic,” explains Dr. Johnson, a chiropractor who treats Medi-Cal patients. “When I see children with scoliosis or sports injuries, I can create a proper treatment plan based on what they actually need, not arbitrary visit limits. Once they turn 21, though, those restrictions kick in.”
Does Medi-Cal Cover Chiropractic Care Without a Referral?
Whether you need a doctor’s referral for Medi-Cal-covered chiropractic care depends on your specific plan.
With standard Fee-for-Service Medi-Cal, you can generally self-refer for chiropractic services without getting your primary care doctor involved first. You’ll still need to receive services at an FQHC/RHC if you’re an adult, but you can initiate care directly.
Managed Care Plans have varying policies. Some require primary care physician referrals, while others offer direct access to their network chiropractors. For example, San Francisco Health Plan members aged 18+ with Medi-Cal can access chiropractic care directly through ASH without a referral by simply calling 1(800) 678-9133 to find a participating provider.
“The direct access was a game-changer for me,” shares James, a Medi-Cal member in San Francisco. “When my neck pain flared up, I just called ASH, found a chiropractor in my neighborhood, and got in within days. No waiting for doctor appointments or referral paperwork.”
If you’re unsure about your plan’s requirements, it’s always best to call your Medi-Cal managed care plan’s member services department. They can explain your specific coverage and referral needs, potentially saving you time and frustration.
Limits, Exemptions & Authorization
Navigating Medi-Cal’s chiropractic rules might feel like solving a puzzle, but understanding the limits and exceptions can help you access the care you need without unexpected bills.
For most adults on Medi-Cal, the standard limit is two chiropractic services per calendar month. This rule comes straight from California Code of Regulations Title 22 §51304(a). Think of it as your monthly chiropractic allowance – once you’ve used your two visits, you’ll typically need to wait until next month for more care.
But here’s the good news: Medi-Cal recognizes that some people need more comprehensive care. Several groups qualify for special exemptions:
| Category | Monthly Visit Limit | Requires FQHC/RHC? | Special Requirements |
|---|---|---|---|
| Standard Adult (21+) | 2 per month | Yes | Services at FQHC/RHC only |
| Children (Under 21) | Unlimited if medically necessary | No | EPSDT coverage |
| Pregnant/Postpartum | More than 2 with authorization | No | Use of TH modifier |
| Nursing Facility Residents | More than 2 with authorization | No | Use of KX modifier |
| Continuing Care After 21 | More than 2 with authorization | No | Use of GY modifier |
When your back pain doesn’t follow the two-visit-per-month schedule (because pain rarely does!), your provider can request additional services by submitting a Treatment Authorization Request (TAR). This form is essentially your chiropractor’s way of telling Medi-Cal, “My patient needs more care, and here’s why it’s medically necessary.”
Getting More Visits When Medically Necessary
“What happens if I need more than two visits in a month?” This is one of the most common questions we hear from patients with Medi-Cal chiropractic coverage.
When your condition requires additional care, your chiropractor becomes your advocate. They’ll need to build a case for why more treatments are medically necessary by:
Documenting your progress with detailed notes showing how the treatments are helping you
Using the right ICD-10 diagnosis codes that match your condition
Creating a clear treatment plan with specific goals
Explaining why stopping at two visits would hinder your recovery
“The key is showing functional improvement,” explains Dr. Thompson, who works with many Medi-Cal patients. “When I request additional visits, I document exactly how the treatments are helping my patient walk farther, sit longer, or return to work. Medi-Cal wants to see that the care is making a real difference in your life, not just temporarily masking symptoms.”
Your managed care plan might have its own process for requesting additional visits, so it’s worth asking your chiropractor or calling your plan directly to understand the specific requirements.
Special Rules for Pregnant Members & Nursing Facilities
If you’re pregnant or living in a nursing facility, Medi-Cal’s chiropractic coverage rules are more flexible for you.
For pregnant individuals, Medi-Cal recognizes that pregnancy creates unique musculoskeletal challenges. The weight of carrying a baby can cause significant back pain and postural changes that chiropractic care may help address. If you’re pregnant, you:
Can receive care beyond the two-visit monthly limit (with proper authorization)
Don’t have to go to an FQHC or RHC for treatment
Remain eligible for this expanded coverage until 60 days after your pregnancy ends
Your provider will need to use a special code (the TH modifier) on your claims to indicate your pregnancy status.
Sarah, who received chiropractic care during her third trimester, found the coverage invaluable: “The lower back pain was making it hard to sleep or even walk. Being able to see my chiropractor weekly made a huge difference in my comfort level. I’m so grateful Medi-Cal covered these visits.”
For nursing facility residents, Medi-Cal also provides expanded access to chiropractic services. If you live in a skilled nursing facility, you can:
Receive more than two treatments monthly when medically necessary
Have the chiropractor come to you at the nursing facility
Avoid the FQHC/RHC requirement that applies to most adults
Your provider will use the KX modifier on claims to indicate your nursing facility status.
These special exemptions recognize that certain groups have unique needs that may benefit from more consistent chiropractic care. If you fall into one of these categories, be sure to discuss your coverage options with both your chiropractor and your Medi-Cal plan.
Covered vs. Not Covered Services & Billing Codes
Navigating what Medi-Cal covers for chiropractic care can feel like solving a puzzle. Let’s break it down in simple terms so you know exactly what to expect at your next appointment.
When Medi-Cal agrees to pay for your chiropractic care, they’re really only covering one main thing: manual manipulation of your spine. These are identified by three specific billing codes:
- 98940: Manipulation of 1-2 spinal regions
- 98941: Manipulation of 3-4 spinal regions
- 98942: Manipulation of all 5 spinal regions
Your chiropractor needs to connect your treatment to an approved diagnosis code that shows your care is truly necessary—not just something that might feel good. The diagnosis must show a clear relationship between your spine issues and the symptoms you’re experiencing.
“I was confused about why Medi-Cal would cover one treatment but not another,” shares Miguel, a Medi-Cal patient from Sacramento. “My chiropractor explained that they’re really focused on just the hands-on spinal adjustments—nothing fancy or extra.”
What you won’t find covered are services like X-rays ordered by your chiropractor (though they might be covered if your regular doctor orders them), massage therapy, or acupuncture performed by your chiropractor. Medi-Cal also won’t pay for “maintenance” adjustments—those preventative visits when you’re not actually having symptoms.
Those special tools or devices your chiropractor might use during your adjustment? Those aren’t separately billable either. They’re considered part of the main service.
For a deeper dive into typical costs associated with chiropractic care, Veeva Clinics offers a helpful cost breakdown on their website.

What Documentation Does Medi-Cal Require?
Paperwork matters—a lot—when it comes to getting Medi-Cal to cover chiropractic care. Without the right documentation, you might end up with a denied claim and an unexpected bill.
Every visit to your chiropractor should generate detailed progress notes that document your complaints, what the chiropractor found during examination, their assessment of your condition, the treatment plan, and how you responded to treatment.
The diagnosis documentation needs to clearly show the connection between your diagnosis and symptoms, with evidence of spinal misalignment or other covered conditions, and how these problems are limiting your daily activities.
When it comes to billing, there are specific codes your provider needs to use. If you’re receiving care at an FQHC or RHC, they’ll need to use Place of Service code 50. And if you qualify for an exemption—like being pregnant or living in a nursing facility—they’ll need to add special modifiers to your billing codes.
“The paperwork is honestly the hardest part,” admits Dr. Garcia, who treats Medi-Cal patients in Fresno. “I need to thoroughly document why each adjustment is medically necessary—not just that the patient has pain, but how that pain is affecting their ability to work, sleep, or care for themselves.”
What Medi-Cal Won’t Pay For
Being clear about what Medi-Cal won’t cover helps avoid surprise bills when you’re seeking chiropractic care.
Maintenance care is a big no-no. If you’re feeling great and just want an adjustment to stay that way, Medi-Cal won’t cover it. Your treatment must address active symptoms and functional problems—not just preventative care.
Unlike some insurance plans, Medi-Cal doesn’t pay for separate examination codes when they’re billed alongside adjustment codes. They consider the evaluation part of the adjustment service.
Experimental therapies without proven effectiveness aren’t covered either. This includes some newer chiropractic techniques that haven’t yet established their efficacy through research.
Beyond basic spinal manipulation, many therapies commonly offered in chiropractic offices won’t be covered. This includes electrical stimulation, ultrasound, heat or cold therapy, therapeutic exercises, and massage therapy—even if they might help your condition.
Sophia, who receives Medi-Cal benefits in Oakland, learned this the hard way: “My chiropractor recommended some electrical stimulation to help with my muscle spasms. I assumed it would be covered like my adjustment was, but I ended up with a bill. I wish I’d known to ask about coverage before agreeing to the treatment.”
If you need services that aren’t covered by Medi-Cal, talk openly with your provider about payment options. Many offer sliding-scale fees or payment plans for patients who need care beyond what their insurance covers.
Finding a Medi-Cal Chiropractor & Comparing Insurance Options
Finding a chiropractor who accepts Medi-Cal can feel like searching for a needle in a haystack, especially with the FQHC/RHC requirements and limited reimbursement rates. But don’t worry – you have several options to help you connect with the care you need.
For most adult Medi-Cal members, your chiropractic care will need to come through one of these settings:
Federally Qualified Health Centers (FQHCs) provide community-based healthcare to underserved populations. These centers receive federal funding specifically to help patients like you access essential services, including chiropractic care in many locations.
Rural Health Clinics (RHCs) offer similar services but focus on rural communities where healthcare access might otherwise be limited. If you live in a rural area, these clinics might be your best option.
Managed Care Network Providers may be available if you’re enrolled in a Medi-Cal managed care plan with expanded chiropractic benefits. Some plans have special arrangements that give you more options than standard Medi-Cal.
“When I first needed chiropractic care, I had no idea where to start,” shares Elena, a Medi-Cal member in Fresno. “My managed care plan connected me with an ASH network provider just 10 minutes from my home. I was surprised how easy it was once I knew where to look.”
To locate these providers, you have several helpful resources:
- Use the HRSA (Health Resources & Services Administration) data warehouse to find nearby FQHCs through their searchable directory at https://findahealthcenter.hrsa.gov/.
- Call your Medi-Cal managed care plan’s member-services department or check their online directory.
- If your plan contracts with American Specialty Health (ASH), call ASH directly to find participating chiropractors who are ready to serve Medi-Cal members.

What About Medicaid Coverage in Oregon and Washington?
Because Veeva Chiropractic’s clinics are located in Oregon and Southwest Washington, many of our patients use Oregon Health Plan (OHP) or Washington Apple Health rather than Medi-Cal.
• Oregon Health Plan (OHP): OHP covers spinal manipulation when it is ordered or referred by an OHP-enrolled primary-care provider and tied to a covered diagnosis on the Prioritized List of Health Services. Unlike Medi-Cal, there is no fixed “two-visit” cap, but services still need to be medically necessary and properly documented.
• Washington Apple Health: Apple Health currently covers chiropractic manipulation for children under 18, pregnant individuals, enrollees receiving Medicare cost-sharing assistance, and a few other special populations. Adults outside these groups generally pay out-of-pocket unless they have supplemental insurance.
If you have OHP or Apple Health, call the Veeva clinic nearest you and we’ll gladly verify your individual benefits and any referral requirements.
Medi-Cal vs. Medicare vs. Private Insurance (With OHP & Apple Health Call-Outs)
Understanding how Medi-Cal’s chiropractic coverage stacks up against Medicare, private insurance, and other regional Medicaid programs can help you steer your options, especially if you qualify for multiple types of coverage.
| Feature | Medi-Cal | Oregon Health Plan | Apple Health (WA) | Medicare | Private Insurance |
|---|---|---|---|---|---|
| Visit Limit | 2 per month (standard) | No preset cap (must be medically necessary) | Limited to kids, pregnant people, and special groups | No set limit, but must be medically necessary | Varies by plan (often 20-30 per year) |
| Cost to Patient | No cost | No cost | No cost for eligible groups | 20% coinsurance after deductible | Copay ($15-50) or coinsurance (20-50%) |
| Provider Restrictions | FQHC/RHC for most adults | Must be OHP-enrolled provider & referral | Must be Apple Health-enrolled provider | Any Medicare-participating chiropractor | In-network providers for best coverage |
| Referral Required | Varies by plan | Usually yes | Usually yes | No | Varies by plan |
Michael, who qualifies for both Medi-Cal and Medicare, found a silver lining in his dual coverage: “Having both programs works great for my back issues. Medicare lets me see any participating chiropractor, not just those at FQHCs, and Medi-Cal covers the 20% that Medicare would normally charge me. It’s the best of both worlds.”
If you have private insurance, look into whether your plan offers chiropractic riders or supplemental coverage. These add-ons can provide additional benefits beyond your standard plan if you need regular chiropractic care.
How to Verify Your Eligibility and Benefits
Before scheduling your first adjustment, it’s crucial to verify your specific Medi-Cal, OHP, or Apple Health coverage and benefits. Taking this step can prevent unexpected bills and help you access all the services you’re entitled to receive.
Follow these simple steps to confirm your coverage:
- Check your eligibility status through your program’s online portal (e.g., AEVS for Medi-Cal, ONE Account for OHP, or WA ProviderOne for Apple Health).
- Contact your managed care plan or coordinated care organization (CCO). Be specific about chiropractic coverage – ask whether you need a referral and which providers or facilities are covered under your plan.
- Document everything during these conversations. Note the date, time, representative’s name, and any reference number.
If you qualify for an exemption category – like being under 21, pregnant, or residing in a nursing facility – make sure this information is noted in your record and communicated to your provider. These special statuses can significantly expand your access to chiropractic care under any Medicaid program.
Conclusion
Navigating Medi-Cal’s chiropractic coverage – or its Northwest counterparts OHP and Apple Health – might feel like solving a puzzle, but understanding your benefits is the key to getting the care you need for your spine and pain management.
Let’s recap:
• Medi-Cal covers up to two medically necessary spinal-manipulation visits per month for most adults, with broader coverage for children, pregnant people, and nursing-facility residents.
• Oregon Health Plan generally requires a provider referral but does not impose a strict monthly cap when care is medically necessary.
• Washington Apple Health offers chiropractic benefits primarily for children, pregnant people, and a few special populations.
It’s worth noting that all three programs pay only for manual manipulation of the spine – not extras like X-rays or massage therapy. Some managed care plans do offer wider networks through partners like ASH, which might make finding care easier. And if you need more than two visits in a month, there’s a process for that, though it does require authorization.
At Veeva Chiropractic, we understand these complexities and how frustrating they can be. Our clinics in Beaverton, Happy Valley, Hillsboro, Gresham, Portland, Salem, Vancouver WA, and Woodburn work with many insurance plans every day, including OHP, Apple Health, Medicare, and a wide range of private insurers. We’ll happily verify your benefits for you so you can focus on healing.
Chiropractic care offers a drug-free approach to managing spinal conditions that can truly improve your quality of life. Don’t let the complexity of insurance keep you from seeking relief.
For more details about how chiropractic services might help your specific condition, our chiropractic services page has a wealth of information.
While coverage matters, your health matters more. If pain is affecting your daily life, talk with healthcare providers who can help you find the right path forward – one that works for both your body and your budget.